
What is chondromalacia?
The knee joint is composed of three bones:
- The femur (thighbone)
- The tibia (shinbone)
- The patella (kneecap)
In a healthy knee, flexible connective tissue called cartilage coats the end of these bones and a thick liquid lubricates it. This allows for smooth, normal movement.
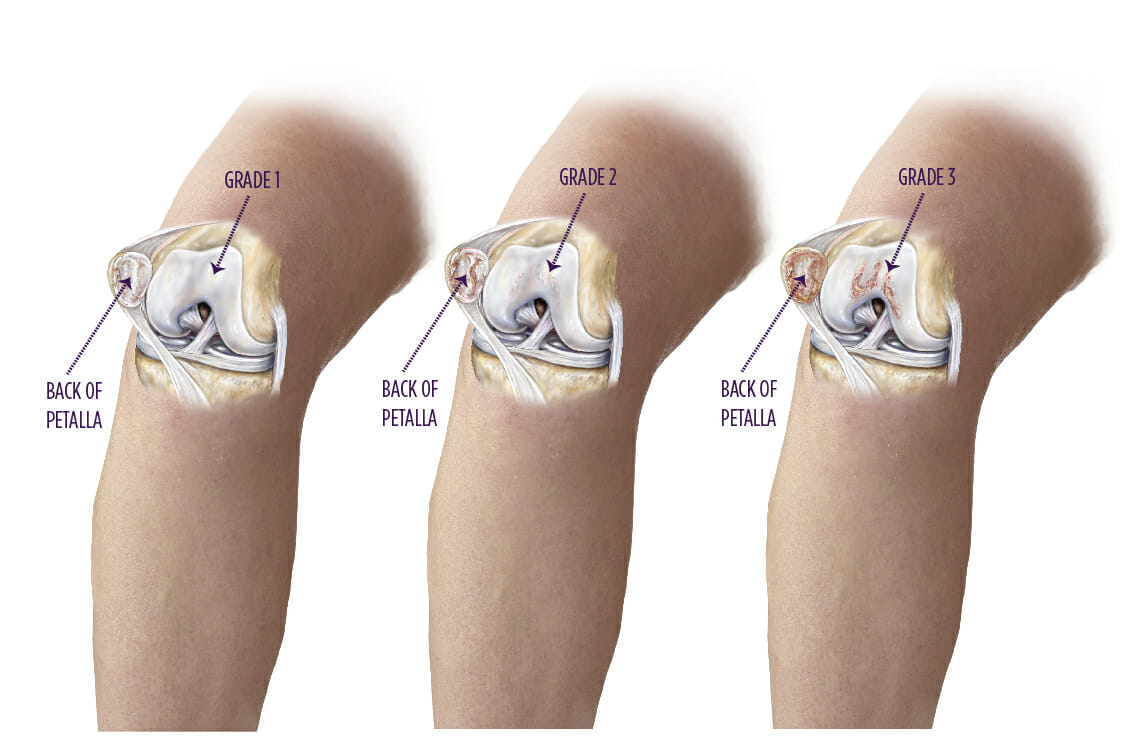
Chondromalacia is a softening and subsequent roughening of the joint’s surfaces. As a result, the bones are not able to move freely and without pain.
What causes chondromalacia?
Chondromalacia is usually associated with injury, overuse of the knee, and poorly aligned muscles and bones around the knee joint. Common causes include:
- Trauma to the kneecap, such as a fracture or dislocation
- Repeated bending or twisting of the knee joint, especially during sports
- Poorly aligned muscles or bones near the knee joint
- An imbalance of the muscles around the knee (some muscles are weaker than others)
- Injury to a meniscus (C-shaped cartilage inside the knee joint)
- Rheumatoid arthritis or osteoarthritis
- An infection in the knee joint
What are the symptoms of chondromalacia?
Symptoms of chondromalacia can vary from person to person and may be mild, moderate, or severe. Common symptoms include:
- Swelling
- Clicking and grinding within the knee
- Pain that is aggravated by squatting, running, and/or using the stairs
How is chondromalacia diagnosed?
Your physician will review your medical history to determine if there’s been a fracture, sprain, infection, or arthritis in your knee that might be a contributing factor. A physical exam will check:
- How well your kneecap aligns with your thighbone
- How well your knee responds to bending and straightening
- How your painful knee compares with your other knee
- If there is swelling, deformity, tenderness, and fluid in the knee join
Diagnostic imaging, such as X-rays or an MRI, may also confirm a diagnosis of chondromalacia.
How is chondromalacia treated nonsurgically?
The goal of treatment is to reduce the pressure on your kneecap and joint.
- Initial treatment may consist of resting, stabilizing, and icing the knee.
- The cartilage damage resulting in runner’s knee can often repair itself with rest.
- Your physician may also prescribe anti-inflammatory medications to reduce inflammation.
- If swelling, tenderness, and pain persist, physical therapy and non-weight-bearing exercises may be recommended, such as swimming or riding a stationary bike.
- More advanced cases may require a cortisone injection or joint fluid therapy, which replaces the natural lubricants found in healthy joints.
What are the surgical treatment options for chondromalacia?
If nonsurgical treatments are not successful, or if you have severe symptoms, your doctor may recommend knee arthroscopy. Arthroscopy is a minimally invasive operation in which the surgeon examines the joint with an arthroscope, a pencil-thin device equipped with a camera lens and light, while making repairs through a small incision. If necessary, your doctor also can correct the alignment of your kneecap or other parts of your knee to help to reduce wear and tear on your knee cartilage.
