Your hips support an active life. If they’re hurting, though, even the most routine activities, such as going for a walk with friends or bending to pick up your grandchild, may become challenging. Hip arthritis is one of the most common causes of hip pain. This disease doesn’t have a cure, but with treatment, you can control the symptoms and continue enjoying the activities that help make you who you are.
The experts at Summit Orthopedics are ready to help people in the Minneapolis/St. Paul area get the diagnosis and treatment you need so you can continue the activities you love.
What Is Hip Arthritis?
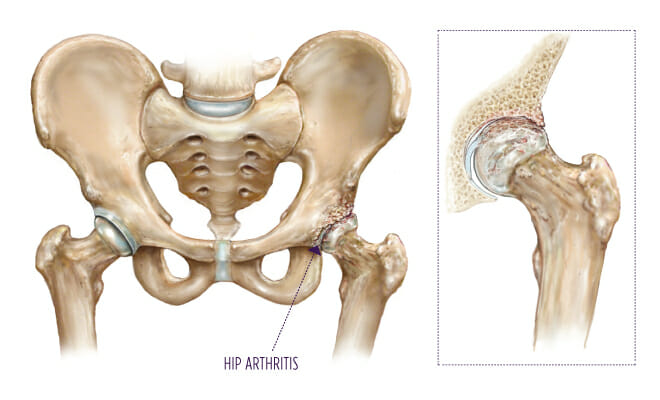
Your hip is a ball-and-socket joint. The top of your thighbone (the ball), which is known as the femoral head, sits within part of the pelvis called the acetabulum (socket). Cushioning, called cartilage, covers the surfaces of these bones, allowing them to move against each other easily. Arthritis, which is inflammation of the joint, can rob it of this cushioning over time.
Several types of arthritis can affect the hips, but osteoarthritis is the most common form. With osteoarthritis of the hip, cartilage slowly breaks down over time, causing pain, stiffness and other symptoms that gradually worsen. Eventually, as cartilage in the hip disappears, the femoral head and acetabulum may rub against each other painfully and form small growths called bone spurs.
What Does Arthritis in the Hip Feel Like?
At first, you’ll likely notice pain and stiffness in your hip with certain movements or at consistent times, such as waking up in the morning, during activity or after sitting for a long period. As hip arthritis progresses, the symptoms usually become more frequent. Pain may occur during periods of rest at night. It may even wake you from sleep. In some cases, discomfort may spread to the groin, buttocks or knee.
In addition to pain, hip arthritis can cause:
- A grinding noise when you move your hip
- Difficulty bending or walking
- Locking of the hip
- Reduced range of motion that may lead to a limp
Hip Arthritis Causes and Risk Factors
With osteoarthritis, changes in the cartilage of the hip cause the tissue to break down over time. Why these changes occur isn’t clear, but several factors can increase your risk. Knowing your risk factors can help you make lifestyle changes that can protect your hips.
These risk factors may contribute to osteoarthritis of the hip:
- Aging: Your cartilage has a harder time healing itself as you get older, which helps explain why osteoarthritis usually develops after age 50.
- An improperly formed hip: If you were born with a condition called developmental dysplasia of the hip, the joint’s ball and socket don’t fit together like they should. This poor fit can increase the risk of osteoarthritis.
- Excess weight: Carrying an unhealthy amount of weight places extra stress on the hips, potentially setting the stage for arthritis.
- Family history: Osteoarthritis can run in families, so you may be more likely to develop it if a parent had it.
- Hip injury: Damage to the joint from an injury can lead to osteoarthritis.
When to See a Physician
If hip pain and stiffness damage your quality of life, don’t delay seeking medical help. The sooner you receive a diagnosis and start treatment, the better you may be able to control hip arthritis as it progresses.
Start by seeing your primary care provider. They may refer you to an orthopedic specialist who can diagnose arthritis and recommend a wide range of treatments. You’ll start with nonsurgical options, and if they don’t provide the relief you’re seeking, you and your orthopedic specialist may discuss a surgical solution.
Diagnosing Hip Arthritis
Your physician will ask about your medical history and symptoms and conduct a physical examination to look for clues that could point to hip arthritis. They will also order diagnostic imaging to look for arthritis-related changes in the hip.
Medical History and Physical Exam
The physician will ask about your health history, including any current conditions you’re managing and how you’re doing so. They will also inquire about your symptoms, including when you first noticed them, what they feel like, how often they occur, what aggravates or improves them, and how they affect your quality of life.
Your physician will conduct a physical exam to assess your health and look for signs of arthritis and hip joint pain. They may feel the joint for tenderness, ask you to walk so they can observe your gait and range of motion, and check for signs of soft tissue injury near the joint.
Imaging Tests
You will have an X-ray to look for changes to the bones that could be due to arthritis, such as bone spurs or narrowing of the space between the ball and socket. Rarely, physicians may order a CT or MRI scan to check the condition of the soft tissues in the hip. In most cases, though, physicians only need an X-ray to diagnose hip arthritis.
Hip Arthritis Treatments
Your orthopedic specialist will help you find a treatment or combination of treatments that allows you to get active again. You’ll start this process by trying conservative, nonsurgical therapies until you find one that works for you. These treatments may include lifestyle modifications, physical therapy, medications and more. Nonsurgical treatments work for many people, but if they aren’t effective for you, surgery, such as total hip replacement, may be the solution you need.
Lifestyle Changes
You can help protect your hips and slow the progression of arthritis by making some healthy lifestyle changes. Try these steps:
- Lose weight to take some of the pressure off your hips and reduce pain.
- Avoid activities that can aggravate hip arthritis, such as climbing stairs and engaging in high-impact exercises or sports that put stress on your joints, like running and soccer.
- Switch to low-impact exercises, such as swimming or walking, that strengthen your hips and can help relieve symptoms without contributing to cartilage breakdown.
Physical Therapy
A physical therapist can teach you exercises to improve your hip’s strength, flexibility and range of motion. You’ll have several sessions with your therapist, and you’ll be able to continue your exercise program at home long after therapy ends to maintain and build on its benefits.
Medications
Several over-the-counter medications are available to reduce pain, inflammation and other symptoms. These include acetaminophen and a class of medications called nonsteroidal anti-inflammatory drugs, or NSAIDs, such as ibuprofen. If over-the-counter therapies don’t work for you, your physician may suggest a prescription pain reliever.
Injections
Corticosteroid injections, which involve injecting anti-inflammatory medications into the joint, help many people with hip arthritis find relief. Your physician can prescribe this treatment.
Assistive Devices
Hip joint pain can reduce your mobility, making it difficult to get around the grocery store or even your home. Your physician may recommend using a cane or walker to make moving easier.
Surgery
For severe arthritis or symptoms that don’t improve with nonsurgical treatments, surgery may offer the best chance of controlling or eliminating symptoms and getting back to an active lifestyle.
Your orthopedic specialist may recommend total hip replacement, a procedure in which the surgeon removes the damaged ball and socket bones and replaces them with artificial components, such as metal or plastic. Modern hip replacement procedures are significantly gentler, and the techniques surgeons use minimize damage to the surrounding muscles. This helps you recover faster, move around sooner and have fewer limits after the procedure.
Find your Summit Orthopedics arthritis care expert, request an appointment or call us at (651) 968-5201 to schedule a consultation.
